Why will cancer be the cause of your death ?
February 5, 2026Chronic diseases like cancer do not develop overnight. In this detailed guide, we look at how subtle, long-term biological imbalances can quietly affect cancer risk, progression, and survival. Factors such as chronic low-grade inflammation, insulin resistance, circadian rhythm disruption, and indoor air pollution show how everyday lifestyle and environmental elements can shape the body’s internal environment over time. The article pulls from research by groups like the World Health Organization and the American Cancer Society.
It examines how metabolic health, immune regulation, hormonal balance, and stress physiology relate to cancer biology. You will learn how diversity in the gut microbiome can affect the risk of colorectal cancer, how nighttime blue light exposure can suppress melatonin and impact hormone-related cancers, and why maintaining muscle mass through strength training can lower cancer mortality. The article also covers new topics, including exposure to microplastics, optimizing vitamin D, intermittent fasting during chemotherapy, and the role of early palliative care in improving survival outcomes.
This post also points out the strong impact of psychological resilience, social connections, breathing practices, and meditation on immune function and recovery. It stresses that while no single habit can prevent or cure cancer, creating a balanced internal environment through nutrition, sleep, exercise, stress management, and medical support can significantly affect long-term outcomes. This blog is perfect for those looking for science-based, holistic insights into cancer prevention, treatment support, and survivorship. It connects modern oncology with lifestyle medicine, offering practical, evidence-based strategies to help reduce risk, improve treatment tolerance, and support overall well-being.
Hidden Factors That Influence Cancer Risk, Tumor Growth & Survival
Table of Contents
1. How does chronic low-grade inflammation silently raise the risk of cancer over years?
Chronic low-grade inflammation is a chronic immune response that persists quietly in the body without any apparent symptoms. Over the years, the immune cells involved in the inflammation will release chemicals such as cytokines and free radicals, which can damage the DNA and the surrounding tissues. As the body continues to repair the damage, the risk of genetic mutations increases. These mutations can lead to uncontrolled cell growth, which is the first stage of developing cancer.
Moreover, chronic low-grade inflammation can create a favorable environment for tumors to develop by encouraging abnormal cell growth, inhibiting the normal death of damaged cells, and inducing the growth of new blood vessels to feed the tumor cells. It can also impair the immune system’s capacity to recognize and eliminate abnormal cells early. Since this process occurs gradually over many years and without any apparent symptoms such as pain, chronic low-grade inflammation can silently increase the risk of cancer.
2. Can improving the diversity of gut microbiomes lower the risk of certain cancers?
Improving the diversity of gut microbiomes can help lower the risk of certain cancers by boosting the body’s immune system and reducing chronic inflammation. A balanced gut microbiome helps the body digest food properly, produces beneficial compounds such as short-chain fatty acids, and helps the body’s immune system function properly. When the body’s gut microbiome is balanced, it can help decrease bad inflammation and prevent the overgrowth of certain microbes that can potentially cause cancer. Studies have shown that a balanced gut microbiome can help lower the risk of certain cancers, such as colorectal cancer, and can also help the body respond to cancer treatments.
3. Can sleeping in complete darkness (melatonin optimization) help in cancer prevention?
Sleeping in complete darkness can help in cancer prevention by optimizing the body’s production of melatonin, a hormone secreted during the night that controls the sleep-wake cycle. Melatonin is not only essential for the sleep-wake cycle but also has antioxidant properties and regulates the immune system and cell growth. The body’s production of melatonin can be inhibited by light exposure during the night, particularly blue light from electronic devices. Inhibition of melatonin production can have adverse effects on the body’s health and increase the risk of cancer. Some studies have suggested that lower melatonin production is associated with an increased risk of cancer, particularly hormone-related cancers like breast cancer.https://youtu.be/BttAtBZeQc4?t=17
Sleeping in complete darkness may not be sufficient to prevent cancer, but it can help in cancer prevention by maintaining a regular sleep schedule avoiding light exposure during the night. This can help in cancer prevention by regulating the body’s hormonal production and reducing inflammation.

4. How does long-term exposure to artificial blue light affect hormone-related cancers?
Long-term exposure to artificial blue light, especially at night from phones, LED lights, and computer screens, can disrupt the body’s natural circadian rhythm by reducing melatonin production. Melatonin is important for regulating hormones like estrogen and for supporting immune function. When melatonin levels remain low for a long time, it can disturb hormonal balance and may increase the risk of hormone-related cancers, such as breast and prostate cancer.
Some studies link disrupted sleep patterns and circadian misalignment to a higher cancer risk, particularly among night-shift workers. Over time, ongoing exposure to blue light at night may also lead to more inflammation and metabolic changes, both of which are connected to cancer development. However, while research suggests a possible link, the relationship is still under investigation, and blue light is not considered a direct cause of cancer on its own. Reducing light exposure at night, using warm lighting, and keeping consistent sleep habits may help protect hormonal health and lower long-term risk.
5. Can regular cold exposure or heat therapy, like sauna use, influence cancer prevention?
Regular cold exposure and heat therapy, such as sauna use, may help with cancer prevention by improving overall metabolic and immune health, but they are not proven methods on their own. Heat therapy, especially sauna use, can boost circulation, promote detoxification through sweating, lower chronic inflammation, and support heart health. Some studies suggest that repeated heat exposure may activate heat shock proteins, which help protect cells from stress and may aid in cellular repair. Lower inflammation and better immune regulation could potentially decrease long-term cancer risk.
Cold exposure, such as cold showers or ice baths, may also lower inflammation, improve insulin sensitivity, and trigger certain immune responses. These benefits can lead to better metabolic balance, which is important because chronic inflammation and insulin resistance are connected to a higher risk of cancer. However, scientific evidence linking regular cold or heat therapy to cancer prevention is still limited. They may enhance overall health as part of a balanced lifestyle that includes good nutrition, exercise, quality sleep, and avoiding harmful habits. https://youtu.be/I6ss5y1WBSc?t=5

6. What role does insulin resistance play in hidden cancer development?
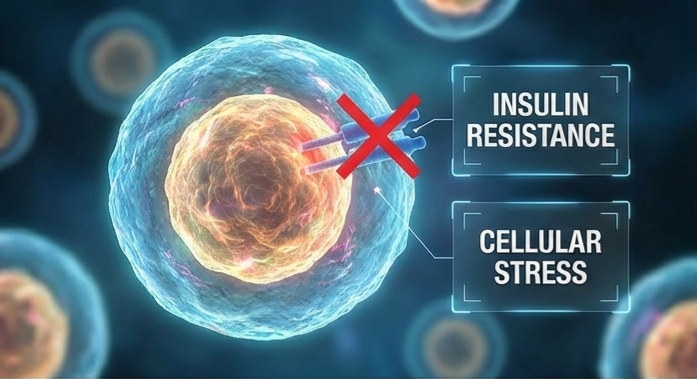
Insulin resistance significantly contributes to hidden cancer development by creating a metabolic environment that encourages abnormal cell growth. When the body resists insulin, it produces higher levels of insulin to make up for it. This condition, known as hyperinsulinemia, can stimulate cell growth because insulin both regulates blood sugar and signals for growth. High insulin levels can activate pathways that cause cells to divide rapidly and resist natural cell death, which increases the chances of mutations accumulating over time.
Insulin resistance is also closely linked to chronic inflammation, obesity, and higher levels of insulin-like growth factor (IGF-1). All these factors may promote tumor growth and progression. These metabolic changes can remain unnoticed for years before cancer becomes detectable. By creating ongoing cellular stress and promoting growth signals, insulin resistance may quietly aid the early stages of cancer development, especially in colorectal, breast, pancreatic, and liver cancers. Keeping blood sugar levels healthy through diet, exercise, and weight management may help lower this long-term risk.
7. Can air pollution inside homes be more dangerous than outdoor pollution for cancer risk?
Yes, indoor air pollution can sometimes pose a greater risk than outdoor pollution when it comes to long-term cancer risk. This is mainly because people spend most of their time indoors. Pollutants can build up in poorly ventilated areas, leading to constant low-level exposure. Common indoor sources of cancer-related pollutants include tobacco smoke, radon gas, cooking fumes, mold toxins, burning solid fuels, incense, and volatile organic compounds (VOCs) from paints, furniture, and cleaning products.
Since indoor air does not flow as openly as outdoor air, harmful particles and gases can reach higher concentrations over time. Long-term exposure to certain indoor pollutants, such as radon and secondhand smoke, is closely linked to lung cancer. In some areas, using biomass fuel for cooking is a major risk factor for respiratory cancers. While outdoor air pollution is also a serious issue, indoor exposure can be more intense and longer-lasting, especially in homes with poor ventilation. Improving air flow, using clean cooking methods, avoiding indoor smoking, and testing for radon can significantly lower cancer-related risks inside the home.
8. How does emotional trauma or chronic stress biologically influence tumor growth?
Emotional trauma and chronic stress can influence tumor growth by disrupting the body’s hormonal and immune balance over long periods. When a person experiences ongoing stress, the body continuously releases stress hormones like cortisol and adrenaline. While these hormones help in short-term emergencies, prolonged elevation can weaken the immune response, reducing the body’s ability to detect and destroy abnormal or pre-cancerous cells. Chronic stress can also increase inflammation, creating a tissue environment that may support cancer development and progression. Additionally, stress-related hormones can activate signaling pathways that promote cell survival, blood vessel formation, and tumor spread.
Long-term stress may also affect behaviors such as sleep quality, diet, and physical activity, which can indirectly raise cancer risk. Although emotional trauma alone does not directly cause cancer, persistent psychological stress can lead to biological changes that may support tumor growth over time. Managing stress through mindfulness, social support, exercise, and healthy coping strategies may help protect overall health and immune function.
9. Are microplastics in food and water a long-term cancer risk?
Microplastics in food and water are becoming a growing concern in science, but we do not fully understand their long-term cancer risk. Microplastics can enter the body through drinking water, seafood, salt, and packaged foods. Some researchers are worried that these tiny particles may carry harmful chemicals like bisphenol A (BPA), phthalates, or other additives that disrupt hormones. Certain chemicals from plastics have been linked to inflammation, oxidative stress, and possible DNA damage, which can contribute to cancer development. However, current evidence does not clearly show that microplastics directly cause cancer in humans.
Most studies are still in their early stages, and there is limited long-term data on humans. Scientists are actively studying how microplastics build up in tissues and how they may interact with cells over time. While the direct link to cancer is still unclear, reducing plastic exposure, such as avoiding heating food in plastic containers, using filtered water, and opting for fresh foods over heavily packaged ones, may help lower potential health risks.

10. Can maintaining muscle mass with strength training lower cancer mortality rates?
Maintaining muscle mass through regular strength training may help lower cancer mortality rates by improving overall metabolic and immune health. Higher muscle mass is linked to better insulin sensitivity, lower chronic inflammation, and improved hormonal balance. These factors all play roles in cancer progression. Muscle tissue also serves as a metabolic reserve during illness, helping the body better handle treatments like chemotherapy and reducing the risk of severe weight and strength loss, known as cachexia.
This condition is associated with poorer outcomes in cancer patients. Research shows that people who regularly participate in resistance training tend to have lower overall mortality rates, including deaths related to cancer. Strength training can boost immune function, reduce fatigue during treatment, and improve quality of life. While it does not prevent cancer by itself, maintaining healthy muscle mass seems to support the body’s resilience. This may lead to better survival outcomes when paired with other healthy lifestyle factors like balanced nutrition, adequate sleep, and regular medical care.
11. How does mindset and psychological resilience affect cancer survival rates?
Mindset and psychological resilience can influence cancer survival rates by affecting both biological and behavioral factors. A resilient mindset helps reduce chronic stress, which lowers prolonged exposure to stress hormones like cortisol. High levels of stress hormones over time can weaken immune function and increase inflammation, both of which may influence tumor progression. Patients who maintain emotional stability and coping skills often show better immune regulation and improved overall physical recovery during treatment. Aloe Vera and Basil: Why These Plants Are Superfoods for Your Body
Psychological resilience also affects survival indirectly through behavior. Patients with a positive and determined mindset are more likely to follow treatment plans, attend regular medical appointments, maintain healthy eating habits, stay physically active, and seek social support. These behaviors can significantly improve treatment outcomes and quality of life. While mindset alone does not cure cancer, strong psychological resilience may improve the body’s response to treatment and contribute to better long-term survival outcomes.
12. Can intermittent fasting improve chemotherapy effectiveness?
Intermittent fasting may improve chemotherapy effectiveness in some cases, but research is still ongoing and it is not a standard medical recommendation. Some early studies suggest that short-term fasting before chemotherapy could make cancer cells more vulnerable to treatment while protecting healthy cells. This happens because normal cells might enter a protective “maintenance mode” during fasting. At the same time, cancer cells, which depend on constant growth signals, may become more sensitive to chemotherapy drugs. Fasting may also lower insulin and growth factor levels, reduce inflammation, and affect metabolic pathways that tumors rely on.
However, clinical evidence in humans is still limited, and fasting during cancer treatment can pose risks, especially for patients who are underweight, weak, or at risk of malnutrition. Since keeping up strength and proper nutrition is essential during chemotherapy, any fasting plan should only be considered with medical supervision. While it shows promise, intermittent fasting is still under investigation and should not replace standard treatment plans.
13. Does maintaining social connection improve survival outcomes in cancer patients?
Yes, keeping strong social connections can improve survival outcomes in cancer patients, both directly and indirectly. Social support helps lower chronic stress, anxiety, and depression. This reduction leads to lower stress hormone levels and less inflammation. Healthier emotional states are linked to better immune function. This function is important for how the body responds to cancer and its treatment. Patients who feel supported often report better sleep, a more positive mood, and greater physical stamina during therapy. Social connection also improves survival through practical and behavioral factors.
Patients with supportive family, friends, or community networks are more likely to go to medical appointments, follow treatment plans, eat well, and stay active. Emotional encouragement can boost motivation and commitment to treatment. These factors are vital for better outcomes. While social support alone does not cure cancer, strong relationships can greatly improve quality of life and may lead to better long-term survival.

14. How does circadian rhythm alignment affect tumor progression?
Circadian rhythm alignment, which means keeping the body’s internal clock in sync with natural day and night cycles, plays a key role in regulating hormones, immune function, metabolism, and cell repair. When this rhythm gets disrupted by irregular sleep, shift work, or exposure to light at night, the production of important hormones like melatonin can drop. Melatonin has antioxidant and anti-inflammatory effects, and it helps control cell growth. Lower melatonin levels and a disrupted hormonal balance may create conditions that let abnormal cells grow more easily.
Circadian disruption can also impact genes that manage the cell cycle, DNA repair, and programmed cell death (apoptosis). When these protective systems fall out of sync, damaged cells might survive and multiply instead of being fixed or removed. Research shows that long-term circadian misalignment is linked to a higher risk and possibly faster progression of certain cancers. Keeping regular sleep patterns, reducing light exposure at night, and matching daily routines with natural daylight may support cellular health and potentially slow down tumor progression as part of a healthy lifestyle.
15. Can personalized nutrition based on genetic testing improve survival chances?
Personalized nutrition based on genetic testing could improve survival chances, but it depends on how the information is applied and the type of cancer involved. Genetic testing can show differences in how a person processes nutrients, responds to inflammation, manages toxins, or regulates blood sugar. In theory, adjusting diet plans to fit these genetic factors might help lower inflammation, improve metabolic health, and support immune function, which are all crucial during cancer treatment and recovery.
However, while precision oncology—testing tumors genetically—is well-established for guiding cancer treatment, nutrition plans based only on inherited genetic testing are still developing. Current scientific evidence shows some promise but limited proof that gene-based diets directly improve cancer survival rates. The most significant survival benefits still come from balanced nutrition, keeping muscle mass, managing blood sugar, and supporting treatment tolerance. Personalized nutrition may improve overall health and treatment response, but it should complement medical care and be guided by healthcare professionals instead of replacing standard therapy.
16. What role does vitamin D optimization play during cancer treatment?
Vitamin D optimization during cancer treatment may support immune regulation, control inflammation, and improve overall treatment response. Vitamin D helps regulate immune cells, supports healthy cell differentiation, and may impact how cancer cells grow and divide. Some studies have linked low vitamin D levels with poorer outcomes in certain cancers, including colorectal, breast, and prostate cancer. Maintaining adequate levels may strengthen immune function and reduce excessive inflammation, which can be beneficial during treatment. Vitamin D may also improve muscle strength, support bone health, and reduce fatigue.
These are important factors for patients undergoing chemotherapy, radiation, or hormone therapy. However, while keeping sufficient vitamin D levels is generally recommended for overall health, high-dose supplementation has not been proven to cure cancer or dramatically improve survival on its own. Vitamin D optimization should be based on blood testing and guided by a healthcare provider to ensure safe and appropriate levels during treatment.
17. Does reducing sugar intake actually slow cancer growth?
Reducing sugar intake does not directly “starve” or cure cancer, but it may help slow cancer growth indirectly by improving the body’s metabolic environment. Cancer cells use glucose (sugar) for energy, but healthy cells do too. So, completely eliminating sugar cannot selectively stop tumor growth. However, high sugar intake can lead to insulin resistance, higher insulin levels, and increased inflammation. Since insulin promotes growth, consistently high insulin levels may create conditions that support tumor progression over time.
Lowering added sugar consumption can improve blood sugar control, reduce excess body fat, and decrease systemic inflammation, all of which are linked to better overall cancer outcomes. A balanced diet focused on whole foods, fiber, healthy fats, and enough protein is more beneficial than strict sugar restriction. While reducing sugar alone is not a standalone treatment for cancer, keeping blood glucose stable and maintaining metabolic health may support the body during cancer prevention and therapy.
18. How does physical activity during treatment influence recurrence rates?
Physical activity during cancer treatment can positively impact recurrence rates by improving immune function, reducing inflammation, and improving metabolic health. Regular exercise helps control insulin levels and decrease excess body fat, both of which are connected to cancer growth and recurrence. It also boosts circulation, which enhances the flow of oxygen and nutrients to tissues. This may help the body handle treatments like chemotherapy or radiation more effectively. These physical benefits can create a less favorable environment for cancer cells to return or grow. Additionally, exercise supports muscle mass, lowers treatment-related fatigue, and improves mental well-being.
This can lead to better adherence to therapy and the development of long-term healthy habits. Research shows that moderate physical activity is linked to lower recurrence rates in some cancers, especially breast and colorectal cancer. While exercise alone does not completely remove the risk of recurrence, maintaining regular, medically supervised physical activity during and after treatment can significantly improve long-term outcomes.
19. Can breathing techniques or meditation affect immune response in cancer patients?
Yes, breathing techniques and meditation can positively influence immune response in cancer patients by mainly reducing chronic stress. Ongoing stress raises cortisol and other stress hormones, which can weaken immune function and increase inflammation. Mindfulness meditation, slow breathing exercises, and relaxation practices help lower stress hormone levels, improve balance in the autonomic nervous system, and reduce inflammatory markers. This can support healthier immune regulation during treatment.
Research shows that mind-body practices may increase natural killer (NK) cell activity, improve mood, boost sleep quality, and reduce anxiety and fatigue; all are important for patients undergoing cancer therapy. While breathing techniques and meditation cannot cure cancer or replace medical treatment, they can act as supportive therapies that strengthen emotional resilience and may improve immune function and overall quality of life during treatment.
20. How does early palliative care improve overall survival, not just comfort?
Early palliative care can improve overall survival by supporting patients physically, emotionally, and medically from the time of diagnosis rather than waiting until later stages of illness. By managing symptoms such as pain, fatigue, nausea, and depression early, patients can often tolerate and continue cancer treatments without interruptions or severe complications. Effective symptom control reduces hospital stays, improves nutrition and physical strength, and helps maintain immune balance.
All of these factors can positively impact treatment results. Early palliative care also improves communication between patients and healthcare providers. This leads to better-informed decisions and more suitable treatment plans. As a result, integrating palliative care with standard cancer therapy can enhance both quality of life and, in some cases, extend overall survival.